July 17, 2020
New UW-developed, arrhythmia-visualization device may save lives, prevent strokes and save hospitals money
As a UW Health pediatric cardiac electrophysiologist, Nick Von Bergen, MD, specializes in caring for children with abnormal heart rhythms, making him a highly valued resource who is often consulted after a child comes out of heart surgery – a time when arrhythmias are common and occasionally life threatening.
When a specialist like Von Bergen is called in, he focuses on achieving an accurate, rapid diagnosis with a constant eye on safety. To achieve the best outcome, Von Bergen depends on accurate interpretation of the signals coming from the heart’s electrical activity. Historically, this information is obtained from the bedside monitor or an electrocardiogram (EKG) in which electrodes are placed on the patient’s chest.
Currently the most easily accessible data source, EKG’s fall short of being a “gold standard” for identification of arrhythmias, especially when every minute counts.

“In a typical case, I may be caring for a baby whose heart rate is spiking at 190 after coming out of surgery,” says Von Bergen, “I want to know if that spike is a response to the baby requiring more fluids, or if this is a potentially more serious abnormal heart rhythm we need to address. Unfortunately, bedside monitors are not precise enough and EKGs can take up to 20 minutes to set up. By contrast, a constant stream of real-time accurate data would help us diagnose heart rhythm immediately and treat the child much sooner,” Von Bergen says. “For pediatric and adult patients, having this information can save lives, prevent strokes and reduce hospital expense.”
Another EKG flaw, Von Bergen adds, is that the atrial, or upper chamber heart signals can be very hard to discern compared with the ventricular, or lower chamber heart signals.
“When we rely on bedside monitors,” he says, “discerning accurate atrial signals from an EKG can be like trying to see a small candle burning near a bonfire,” Von Bergen says. “The atrial signals are so small relative to the much larger ventricular signals.”
Alligator Clips, Wires and Duct Tape
Sensing an opportunity for improvement, Von Bergen was confident there had to be a better way to care for his patients. He began by cobbling together alligator clips, wires and duct tape. Calling it a “prototype” would be a stretch, but his instincts were in the right place.
It might be, thought Von Bergen, a good time to reach across the University of Wisconsin-Madison campus for some additional expertise. His first stop was UW’s Biomedical Engineering Department – a resource that he thought could further evolve his invention. Von Bergen also convinced UW School of Business senior lecturer Pete Lukszys of the potential for his idea. In 2017, Von Bergen and Lukszys, along with two Biomedical Engineering students – Matt Knoespel and Phil Terrien – formed a small business called Atrility Medical, to which Lukszys enthusiastically signed on as CEO.
Knoespel and Terrien, who impressed Von Bergen as having “the right stuff” to succeed as medical device designers, impressed Von Bergen with their work ethic, smarts, and desire to create things that help people.
“They also were excited enough about this ‘ground floor’ business opportunity to turn down more lucrative job offers, and we were lucky to have them as our first two full-time employees,” Von Bergen says.
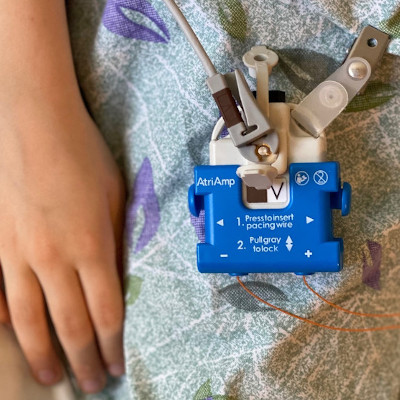
Signature invention named “AtriAmp”
Von Bergen, Lukszys, Knoespel and Terrien – call them the Atrility Four – set out to turn Von Bergen’s original alligator-clip-and-duct-tape prototype into something potentially viable from a clinical, business and engineering perspective.
They designed a device named AtriAmp, short for atrial amplifier, which supports clear, continuous displays of atrial signals in real time.
“AtriAmp’s key feature,” Von Bergen says, “allows epicardial pacing wires, which get temporarily sutured to the heart during surgery, to deliver the highest quality rhythm signal to the bedside monitor, sparing us from reliance on lower quality signals or a long wait for EKG results.”
Early discussions took place with WARF (Wisconsin Alumni Research Foundation), which licenses intellectual property created by UW innovators.
Moreover, UW Health’s Isthmus Project, through its network of clinicians, investors and advisors, connected Atrility’s team with additional support and sources of valuable feedback.
Knoespel and Terrien dedicated themselves full-time to Atrility in 2018 after graduating from UW and spent about 18 months driving the product development. This meant getting up to speed on everything from electrocardiography to the many nuances of interacting with a federal regulatory agency.
“Phil and I appreciate the FDA’s (U.S. Food & Drug Administration) incredibly high bar for safety because of the high-risk situations in which our device will be used,” Knoespel says. “We had to reconsider a lot of things, and we understand why regulation is necessary for a device like this to achieve constant quality and safety.”
More Medical Devices Envisioned
The AtriAmp, just the first of what the Atrility team hopes to be a long line of innovative medical products, has received FDA approval and is expected to begin production by fall of 2020. Manufacturing will take place at a Wisconsin-based contracted manufacturer named Axcesor, located in Grafton, just north of Milwaukee.
“We are very proud that this product will be designed, produced and distributed by Wisconsin people,” Von Bergen says. “It really is a great example of the Wisconsin Idea in which the University seeks to leverage its expertise for the greater good of the state as a whole.”
Lukszys remembers what he told Von Bergen after initially hearing the physician’s presentation for his then-abstract idea for the AtriAmp invention four years ago.
“I said ‘I think you’re on to something, Nick.’ ” Based on how eagerly physicians around the nation are awaiting their device, Lukszys and Von Bergen are on the right track.